If you’ve found this via Google, chances are you’re just like me in 2016 – you’re “terror skimming” for facts. I don’t want to lose you, so I’ll get right to it. Below are 5 absolute necessary things needed to avoid going down the wrong cancer treatment road (I’ll save my reasons why / fun time gifs for the expanded portion below). STRAP IN, HERE WE GO:
1) Get a hard copy of your pathology report. Read it.
2) Ask your oncologist to send off a copy of the pathologist report and slides for a second opinion at a larger cancer hospital.
3) Look up clinical trials to see if you’ll have better odds than the standard treatment you’re offered. This is because…
4) Hospitals cannot tell you if there’s a better treatment offered with better odds elsewhere. Legally they cannot inform you/refer you out so they’ll stick you on their standard of care even if it leads to death.
5) Chemotherapy treatment also differs from hospital to hospital. The chemo regimen most effective for your specific cancer might only be available at certain hospitals.
Above all else, those 5 things are the most important. And you’ve made it here, so you’ve read them all!

You might’ve had questions while reading the top 5 like, “Why?” so now I’ll expand and throw in some bonuses:
1) Ask for your pathology records. Physically read the pathologist’s details. I say this from personal experience. I was told my husband’s cancer was 99% angiosarcoma, yet when I asked for pathology records nearly 3 weeks later (I’ve learned my lesson) the report said “precludes diagnosis”. They weren’t sure at all, but by this point he’d already received 2 cycles of heart toxic chemo for a cancer he never had. Get your eyes on those records!

2) Get a second opinion from a pathologist at a major cancer hospital. You can ask your oncologist to send the biopsy slides to a more experienced pathologist at MD Anderson or Memorial Sloane Kettering. This is free to you. It’s possible they’ll come back with another opinion, like it’s a different cancer or a different staging (which can require a different treatment). If your treatment feels extreme, get a second oncologist opinion.

NOW THAT YOU KNOW YOUR DIAGNOSIS…
Find a cancer specialist. They might have access to clinical trials for your specific cancer. Trials are free to you. On the subject of trials…
3) You can find them here: https://clinicaltrials.gov/
Trials are only offered through certain clinics and institutions so where you’re being treated possibly won’t ever even mention them. Facebook groups for certain cancers are the best place to hear about these trials and see first hand how they’re effective.

4) Many hospitals cannot refer you out, even if they know you have better odds on a treatment that they do not carry. For example, a UC hospital will put you on chemotherapy that only has a 4% survival rate and NEVER tell you there is a trial with an over 50% survival rate offered a 5 block walk away. Cancer patients can be worth millions of dollars to hospitals and they do not want to lose you. Many people feel that by getting a second opinion that they are betraying their doctors. It’s a matter of life and death so don’t be beholden to…

5) Even hospital to hospital, the chemotherapy regimens differ. For example, MD Anderson is the only place that offers HYPER CVAD (because they came up with it). Hyper CVAD has shown the best outcomes for non relapse remission in the cancer Hepatosplenic T Cell Lymphoma (you can find this info in medical paper case studies). This is what led my husband and I from Los Angeles to Houston. If Hyper CVAD performed the best, we’d see if insurance covered and then move to have access to it.

6) If you’re going through a cancer treatment like a stem cell transplant, you may have to deal with many side effects that can be life threatening. These life threatening side effects often have very few treatments (like steroids). Major cancer hospitals will also have access to trial medications for those side effects that other hospitals won’t have access to, like Jakafi. Jakafi is a medication that is still in it’s trial phase for Graft vs Host disease. It saved my husband from death resulting from GVHD – which was a 90% possibility before Jakafi because the other options did not work for him. Getting access to a trial medication like Jakafi is just the first hurdle. Next is insurance. Sometimes insurance covers the cost on the trial medications, but if they don’t you can look into Prescription Partnership, a resource to help with prescription costs: https://www.pparx.org/

7) Pyramid schemes will come out of the wood work offering you miracle cures: Go vegan! Only juice carrots for 3 months! Buy these leaves! Essential oils! No. No. No. Do I believe in supplementing treatment with these things? Sure! But even if someone miracle cured their cancer with only carrots, that is the exception and not the rule. There are too many cancers, too many that are aggressive, and our bodies and these cancers are complexly different. Please do not rely solely on “jacking your immune system” to heal you.
 (the only pyramid scheme I’m interested in)
(the only pyramid scheme I’m interested in)
Do you still feel like something isn’t right? Send me an email, Instagram DM, smoke signal and I’ll do my best to help.
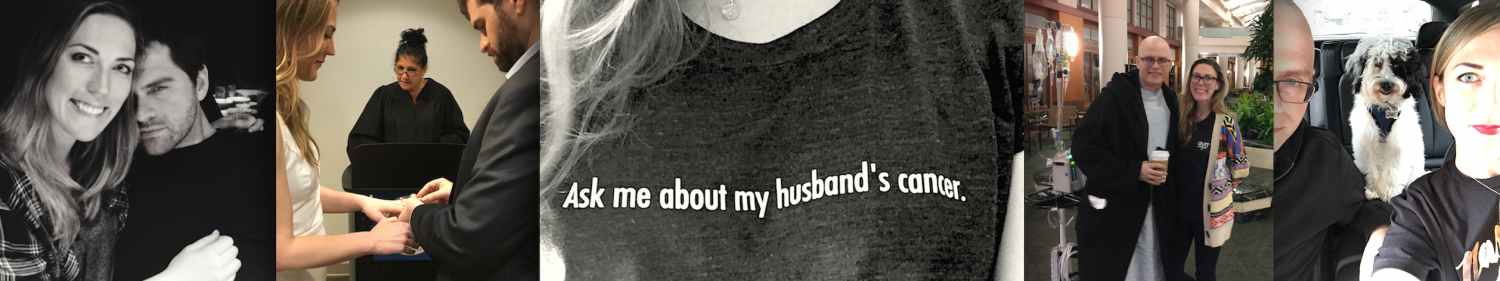


 (me in June of 2015)
(me in June of 2015)



 But, please, with gentle persuasion.
But, please, with gentle persuasion.




 I’m making Jeff a shirt that says’I Survived Cancer and all I got was this Hurricane Harvey T Storm’.
I’m making Jeff a shirt that says’I Survived Cancer and all I got was this Hurricane Harvey T Storm’.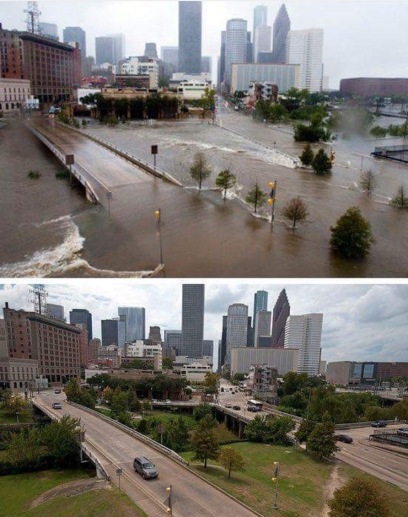
 Stock up on your bartering foods early. This is the selection Target had to offer just 3 days before the storm. Apologies to my mother in law.
Stock up on your bartering foods early. This is the selection Target had to offer just 3 days before the storm. Apologies to my mother in law. 












