https://www.instagram.com/p/BZ-oGPlgBvn/?taken-by=jessicarblackwell
Cancer Doesn’t Evacuate: MD Anderson during Hurricane Harvey

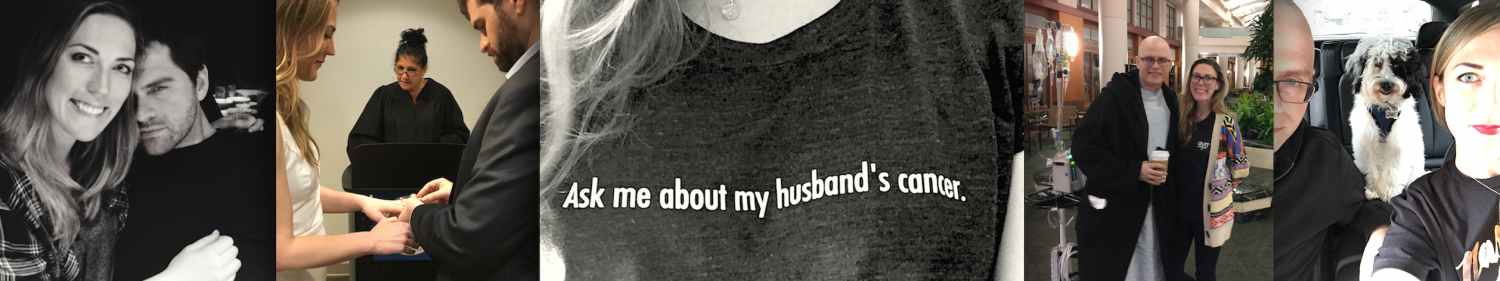
I’d like to start this story off with some good news. The flooding around the hospital finally cleared and I was able to reunite my husband and our dog. You can see their excitement in this video:
https://www.instagram.com/p/BYhTBpnAUu9/?taken-by=jessicarblackwell
My husband and I were on our 50th straight night in the hospital when we heard that Hurricane Harvey, a category 4 hurricane, was barreling towards us in Houston – one of the most flood prone cities in the United States and home of the biggest Medical Center in the world. I guess fighting an extremely rare cancer and nearly going down in an airplane within the last year wasn’t dramatic enough (Lifetime Network, hit me up).
This hurricane felt way too ‘on the nose’. A giant metaphor. Symbolically, a hurricane is a lot like cancer. When you’re told about it, you’re not sure how much damage is coming and you can try to prepare yourself for the overall experience, but only when you’re in it do you finally see all the hurdles that make up the bigger picture. Like…
PAIN
FATIGUE

NAUSEA

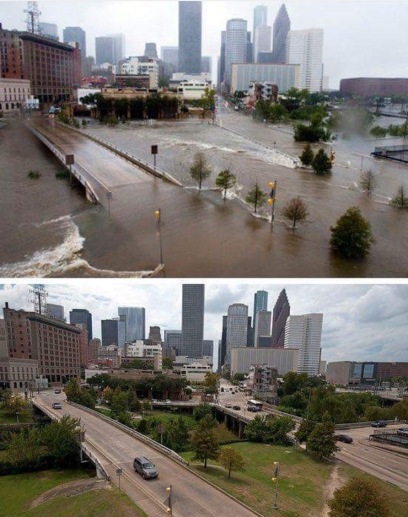
For Houston, the flooding is what truly made Hurricane Harvey terrible. Jeff’s Graft Vs. Host Disease, what we’re inpatient for now, is just like the flooding in that it’s the dangerous after effect that lingers. I’m sure you’ve seen a ton of media coverage on the floods, but here’s some pictures of what the outside and inside of MD Anderson looked like for us on day #1:
Yes, that’s a car flooded and abandoned in front of the hospital. One of many. Some of them positioned as if they were turning into the employee parking lot.
I spent most of the time we were on lockdown scrolling through Facebook and there were a surprising amount of people who thought those who didn’t evacuate were “stupid” and deserved no help. That was when I learned that nothing magnifies rage like cabin fever.
 I’m making Jeff a shirt that says’I Survived Cancer and all I got was this Hurricane Harvey T Storm’.
I’m making Jeff a shirt that says’I Survived Cancer and all I got was this Hurricane Harvey T Storm’.
So let me explain something about evacuations from the point of view of being in this cancer hospital…
If evacuating isn’t mandatory, that means businesses can stay open. Which means hospitals stay open. And, just to reiterate, this medical center is the biggest in the world. That’s a lot of employees (around 106,000) keeping A LOT of people alive.
HERE ARE SOME REASONS WHY STAFF DIDN’T EVACUATE: They were told to come into work and their coworkers and patients were counting on them.
Our night nurse worked 17 hours straight that first night. Nurses normally work on 12 hour shifts and I can only imagine how critical thinking holds up past 12 hours, much less 17. A simple mix up of medications or forgetting to flush a cvc line could mean someone’s life.
The flooding was so bad that nurses were sleeping in shifts of 4 hours in their offices and covering for each other, all while hoping their families and homes were surviving the storm. Eventually water had to be released from reservoirs, threatening even more homes that weren’t originally at risk. One of our nurses was sure it’d flood her house but all she could do was continue her shift and wait and see.
By the second day, a nurse arrived to work in the flooding. Did she kayak in? It was still badly flooded and constantly raining. All of the other nurses on the transplant floor cried when they saw her (I assume partially because they were exhausted and knew she’d provide some relief, but also because they knew how risky it was to try to make it in). Emotions were as high as the water. All sorts of lives were on the line. Doctors couldn’t make it in and were having to review things from home and call in orders.
The hospital was waiting for blood products to be flown in. Transplants could reject without them. On top of that, they were out of coffee. The staff were sleeping in 4 hour shifts on floors with NO COFFEE. It’s amazing how little coffee was available after one single day of lock down. I’m letting you know because if you’re ever in a hospital during a storm, bring coffee to barter with.
 Stock up on your bartering foods early. This is the selection Target had to offer just 3 days before the storm. Apologies to my mother in law.
Stock up on your bartering foods early. This is the selection Target had to offer just 3 days before the storm. Apologies to my mother in law.
HERE ARE SOME REASONS WHY OUTPATIENTS DIDN’T EVACUATE: They could need daily infusions that MD Anderson provides – blood products, platelets, other infusions that literally keep them alive day to day. Do you know how difficult it is to get complete records sent to another hospital while they’re prepping for a hurricane? Do you know how difficult it is to get records sent to another hospital on an average day? Many people travel to Houston for special treatment because it’s one of the few places that handle rare diseases. It’s financially draining to do this, even without factoring in an evacuation.
HERE ARE SOME REASONS WHY OTHER PEOPLE DIDN’T EVACUATE: Some people didn’t evacuate because they don’t have the means. Or maybe because they thought they’d go over to Joel Osteens church and be taken care of there?
I dunno, I think those cover A LOT of people.
As much as I’ve wanted to be out of the hospital and back in the comfort of our apartment over the last couple of months, I feel grateful that we were in MD Anderson during the hurricane. I knew that Jeff was being taken care of. If we had been home and something happened to him, who knows if I’d been able to get him help. But I do know that with the incredible care we’ve been given at MD Anderson over the past year, we would have also chosen to stay. It’s something I think a lot of people outside of the Texas Medical Center fail to think about.
The people of Houston deserve all of the help you can give. Here are a few links to start, and the NY Times link to some additional resources:
The South Texas Blood and Tissue Center is reporting a critical shortage, and has extended hours at all of its San Antonio-area donor rooms. To donate, call 210-731-5590 or visit their website for more information.
Carter BloodCare covers hospitals in North, Central and East Texas. To donate, call 877-571-1000 or text DONATE4LIFE to 444-999.
To help animals suffering from the disaster, visit the Houston Humane Society or the San Antonio Humane Society. The Houston Society for the Prevention of Cruelty to Animals has set up an animal emergency response hotline (713-861-3010) and is accepting donations on its website.
The United Way of Greater Houston flood relief fund will be used to help with immediate needs as well as long-term services like minor home repair. Visit their website to donate or text UWFLOOD to 41444.
Where to Donate to Harvey Victims
Less GVHD, more HGTV (Day +216)

GLOW. It’s a fantastic Netflix series I binge watched the entire first week of July. Little did I know, while I was watching lady wrestlers battling it out in the 80’s, there was a battle going on right next to me…
It was Graft versus Host. Jeff’s New Immune System versus Jeff.

Jeff and I were totally under the impression that we were in the clear by July. The more dangerous stages of GVHD normally occur in the first 100 days and he had avoided it. Or so we thought.
GVHD occurs when immune cells identify the body as something foreign. You actually hope for a LITTLE bit of GVHD, because the cell’s ability to recognize what’s foreign is what fights the cancer. If your new immune system is too similar to your old one, it won’t know to fight the cancer.
This is why GVHD has a higher chance of occurring if your stem cells are from an unrelated donor. Jeff’s stem cells came from his sister, and they were a complete HLA match (jackpot!) but GVHD also has a higher chance of occurring when stem cells are given female to male (or vice versa). ISN’T THIS ALL EXHAUSTING? But wait, theres more:
All allogeneic stem cell transplant patients are given drugs to suppress the new immune system. They’re slowly weaned off so that the cells have time to get familiar with their new body and not attack it. Here’s a gif representation:
IN THE BEGINNING THE CELLS ARE LIKE THIS

BUT AFTER WEANING OFF IMMUNE SUPPRESSANTS THEY CAN GET LIKE

Jeff’s new immune system seems to have qualms with his digestive tract specifically. It’s preventing him from absorbing protein, which didn’t sound so terrible at first – big deal! We’ll go to GNC and get some Muscle Milk, solve this here and now. Except it doesn’t work like that (but I, a non intellectual, was willing to try it). The lack of protein becomes a big problem because protein begets albumin, which is what keeps water in your veins. Without albumin, things (your organs, specifically) can take a quick turn.
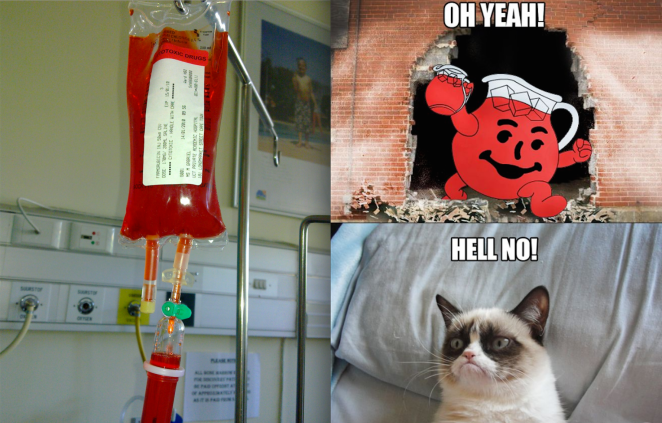
The first thing doctors do when they realize you have GVHD is give you a very high dose of steroids and cross their fingers and hope it works. It only works for about 30% of patients. When that doesn’t work (like it didn’t for Jeff), photopheresis is the next option. Here’s what it looks like:
https://www.instagram.com/p/BXBiz9tBHbH/
The photopheresis machine has a very nonthreatening sound to it – like a Cessna during taking off.
Jeff had a new access line placed into his chest so that they could run his blood through this machine. The photopheresis machine separates the immune system cells and – for lack of a better word – sunburns them so they become less cranky. They then circulate the cells back into his body. He does this 3 times a week, for 2 hours at a time, and it takes weeks to see an effect. This is rough because sometimes the GVHD is so acute that people can’t wait weeks to see results. There has to be something better than this, right?
Enter Jakafi.

Jakafi is the drug’s given name but I prefer to call it Jafar.
Jakafi was originally created for Polycythemia Vera, a slow growing blood disorder. The pill works by lowering your blood cell counts (it’s essentially chemo). Researchers found that it’s effective on some GVHD and so it was approved for off label use only in the last couple of years.
So we waited for the drug manufacturer to approve Jeff’s use of Jakafi, then we had to wait for insurance to approve the cost. This took a week and it often takes much longer. This is a huge issue when each pill costs around FOUR HUNDRED DOLLARS. Jeff takes 4 of these a day. A nurse dropped one on the floor yesterday and I nearly threw up.

Jeff is on day 12 of Jakifi and it can take weeks to work. Each day in the hospital stretches into the next. I find it ironic that the only thing that gets Jeff’s mind off of everything is watching back to back episodes of HGTV shows when we’ve had our fill of acronyms this year.
Every day we risk a life threatening infection by continuing to wipe out his immune system to control the GVHD. Because of this, numerous antibiotics and antifungals are given daily via IV. This puts incredible strain on the kidneys. There has to be perfect balance, so nurses and doctors are working around the clock to keep his body running. It’s a lot like a symphony. The most expensive, anxiety inducing symphony. It’s like the symphony they hired to record the score for JAWS. And for now, all we can do is “wade”* it out.
*I’m so sorry, but not sorry for this.
…and Day +175 post transplant
The ICU

There’s only one thing people want to talk about less than cancer and that’s the ICU. Shortly after my last blog post in February, my husband ended up there. I always thought being sent to the ICU was the “beginning of the end”, but I was wrong. The Intensive Care Unit saved Jeff’s life. Now I want to sing their praises. Literally, with ‘Private Eyes’.
“I.C.U. and you see me… They’re watching you.” How comforting! They’re watching out for you. So closely.
Let me back up and tell you how we got there.
Something no one warns you of is how, post chemo, your veins can get a little…leaky. I don’t want to be too graphic (novel) here but did you see the first X Men movie? Do you remember what Magneto did to Senator Kelly? Do you know how much I hate myself for using this reference? Senator Kelly went from 70-ish% water to 100% water and that was the end of him.
Chemo can cause fluids to go to places they aren’t supposed to go. Sometimes the fluid will cause your legs and feet to swell. It can also end up somewhere dangerous, like in your lungs. Sometimes the water will go straight past your kidneys and your body will believe you’re dehydrated, causing you to drink more water. The cycle continues.
This is what happened to Jeff. He hadn’t been eating well post transplant yet he also hadn’t lost any weight for weeks which was confusing. We didn’t know he was carrying around 20 pounds of water weight around his organs. They warn you that transplant patients can lose or gain weight because of changes in metabolism, so we chalked it up to that. It’s an incredibly insidious thing. More insidious than the amount of Insidious sequels that exist (give it a rest Hollywood). Even now, with Jeff no longer retaining fluid and eating enough to feed a family of four, he’s still losing weight. Most of our conversations are like this now:

So, one morning Jeff wakes me up with chest pain that’s a 5 out of 10 and it quickly progresses to an 8 out of 10 and I call 911. When we get to MD Anderson they do some scans and his lungs are full of fluid. They do a thoracentesis, which is just a Harry-Potter-mythical-creature-sounding word that means they took the fluid out of his lungs. They did this by – how do I explain this technically – punching a hole in his back and putting a suction tube in it. They got a couple of liters (!!) out and he was able to breathe without the chest pressure… temporarily.
That’s when his lab results showed abnormal kidney function. It suddenly plummeted. Our doctor came in to tell us he’d like to send us to the ICU but that it was “precautionary” – not that he needed it immediately, but better safe than sorry. I remember thinking, “this is what they tell everyone I bet”. I was numb. Jeff wasn’t protesting. I knew that was a bad sign.
Let me be honest – the walk to the ICU feels BLEAK. It’s always tucked away from the higher traffic floors. There’s even a special elevator to get to them. There are less windows, if any. The rooms are small and cramped with all sorts of machines. There’s only a recliner, unlike on the regular floors there’s at least a bench to sleep on. I’m actually still confused by this, considering the ICU seems like the place you’d be much more likely stay overnight as a caretaker.
As a side note: I am a terrible sleeper and I can’t sleep unless I’m completely flat. In the ICU I ended up shoving my suitcase in between the recliner portion and the ottoman so I could lay down. It worked perfectly. I highly recommend.

It was around midnight when they transferred us and I couldn’t help but pay attention to every single detail. Patients hooked up to breathing machines, unable to move. The doctor asked me to go to a waiting room while Jeff had an arterial blood pressure line placed in his wrist. It seemed painful and he seemed so out of it (they wouldn’t give him pain medication for fear his blood pressure would get dangerously low). I was so worried that I lasted in the waiting room for about 10 minutes before I was right back outside of his room. He could look out at me through the glass doors while they did the procedure, but I knew I was blurry to him without his glasses on. I just kept making a heart with my hands at him like I was in a stupid Taylor Swift music video.

It was all I could do and I LOST IT. I moved around the corner where Jeff couldn’t see my blurry figure and collapsed on the floor. His nurse happened to just be coming out of the room to check on the dialysis machine when he saw me. He stopped, knelt down and said, “Everything is going to be okay”. He got right back up, helped me into the room, and then assisted another nurse in lining up the 100 or so clear bags needed for the dialysis machine (I wish I could explain what these were for, but I have no idea. Still today I’m convinced dialysis machines run on magic).
I found the nurses in the ICU to be the most empathetic, strong, tactful people in the hospital. They were always aware, walking a fine line with their interactions: not too jovial because the place is a constant reminder that people die, but also not despondent because people are trying to cling to any trace of hope. This just a small layer on top of their many daily actions that make a difference between life and death.
I don’t know how much time I spent thinking about the lives of ICU nurses. It’s amazing what the brain does when simultaneously in trauma and void of stimuli. I don’t even remember Jeff looking as sick as he did at the time. I was like the Shallow Hal of health. I’m pretty sure this was my brain’s way of protecting itself.

Jeff remembers very little of any of this. I had spent most of my time worried about the amount of pain he was in to later find out that his brain was also protecting him. The extreme stress on his mind and body took him to a dream like state where all he remembers is thinking he was on a train with me.
Over the next two weeks Jeff had:
- a groin catheter placed for dialysis
- a drain placed in his heart for pericarditis
- his picc line replaced
- an endoscopy and biopsy to check for GVHD
- around the clock breathing treatments

I made a lot of Top Gun references. It was my excuse to call him Goose.
After his kidneys normalized, we were transferred back to the transplant floor where we spent another two weeks. We were discharged from the hospital in mid March after a full recovery. What transpired was something known as Multisystem Organ Failure and when it happens after transplant it is, more often than not, the cause of mortality. We’d been on the lookout for something like sepsis, not something as simple as excess fluid. We now know how important it is to carefully monitor fluid intake and output after chemo, but especially after myeloablative conditioning.

Jeff and I celebrated with a big ceremony on May 13th – it was the goal line we’d set at the start of transplant. Because of MD Anderson’s ICU team’s care, we made it. We are day +160 post transplant.
THIS IS +40: Life After Allogeneic Stem Cell Transplant

My husband has reached day +40 after allogeneic stem cell transplant. We’ve spent almost the entire last 2 months in the hospital and now we finally get to go home! Time to taste that sweet, sweet freedom.

WELCOME TO OUR NEW SCHEDULE
8:00am – I walk the dog and make some coffee that tastes like 40% creamer and 60% George Michael’s 1990 hit FREEDOM.
8:30am – I administer my husband’s first medication, Cellcept (to prevent Graft Versus Host Disease), which has to be taken on an empty stomach. I also wait an hour to eat breakfast because I’m not a monster. My husband’s body is hurting and he can barely walk thanks to the conditioning chemo he had weeks and weeks ago, so I run him a bath. Other than hard drugs equivalent to heroin, this is the only thing that seems to help.
9:00am – I feed the dog. I get the first “What’s the update???!!??” text of the day. I throw my phone in the trash. I help Jeff get out of the bath since he’s on Lovenox blood thinners so if he fell thanks to the neuropathy and hit his head, he’d die. Baths are super stressful now. Speaking of Lovenox, time for the first Lovenox injection of the day! And breakfast. And then more pills…
10:00am – breakfast is finished. Time for the pills that need to be taken on a full stomach: Gabapentin (for his nerve pain), Protonix, Tacrolimus (both of these are drugs to prevent GVHD), Ibuprofen, and CMV med infusion (to prevent a virus rearing it’s ugly head). I have to wear 2 pairs of gloves when giving him the CMV meds because it absolutely CANNOT touch my skin, even though I am injecting it into his body. I know they are very serious about this because I had to take a long class on how to do it properly and the meds are stored in a bright yellow bag marked CHEMO that is currently in my fridge surrounded by all the foods I’ll eventually digest. This seems super safe. And CRAAAAP and I was supposed to take the CMV meds OUT OF THE FRIDGE 2-4 HOURS AGO to give it time to reach room temp. I take it out of the fridge. I’ll just have to do the CMV infusion at the hospital. We have daily 5 hour outpatient infusion appointments so Jeff can get the rest of the meds they don’t trust me with, even when double gloving it.

(basically me and Jeff twice a day)
10:30am – I walk the dog again and shove an oatmeal cream pie into my stupid face.
10:50am – I can hear our dog Yelp from inside our apartment as Jeff shuffles down our apartment complex’s hallway. It’s the longest hall of all time to get to our parking garage. Why didn’t I think about this when we moved in!? Where can I steal a wheelchair? I’ve decided that next time I’ll roll him down to the car in our computer chair.
11:15am – We pull into MD Anderson and the closest parking garage is FULL. We’ll be late for our appointments if we spend 20 minutes looking for parking so we valet it and grab a super convenient (and pink) wheelchair. Also it’s Wednesday, and on Wednesdays we wear pink. Can’t wait to get home after this, maybe I’ll relax and watch Mean Girls!
11:30am – We make it just in time for the 11:30am blood draw appointment. We check in on the computer and wait to be called.
11:45pm – My husband’s blood is drawn. They realize one of his PICC lines is clogged. He’s had issues with blood clots before so after our infusion appointment, we’ll need to go see the IV team.
12:00pm – I push Jeff’s wheelchair up to the 10th floor to wait for our infusion appointment. The lab is behind today, so Jeff falls asleep in his chair as I grab a grande Caramel Machiatto for my stupid face.

(when I see this I think, Tuffy the Satire Slayer)
1:00pm – I’ve finished my coffee and I’m looking at memes on my phone like a 12 year old boy when we’re called back. Jeff’s vitals are taken, his heart rate is better than it’s been in a week. I feel a sense of victory, like I’m somehow responsible. We’re led into our own room for infusion time.
1:20pm – Jeff settles into bed and I take my seat in what has the comfort level of a high school homeroom class chair. His lab work print out is brought in. His hemoglobin is on the upswing. Jeff looks GREAT on paper but unfortunately still feels like crap in real life. I take out my laptop and check my emails before realizing I forgot a prescription that needs to be picked up at the pharmacy. Feeling super lucky today because the pharmacy just also happens to be on the 10th floor! I love that because this place is huge and I’m ready to be lazy.
1:45pm – I’m waiting at the pharmacy. Turns out his preventative anti fungal is NINE THOUSAND DOLLARS. That’s right, $9,000.00. Even with running Jeff’s Blue Shield insurance it would cost hundreds and hundreds of dollars for a month supply. I’m given a coupon to use with it and, once they can get them to approve it, I’ll have to pay only $100. I listen to an elderly woman next to me be told her insurance doesn’t cover a lot of her meds and that her total is $22,000. Fired up on espresso and rage, I start to understand the concept of suicide bombings.
2:45pm – After nearly an hour wait for pharmacists to talk to Blue Shield (which I am v grateful for), I have the 2008 Toyota Prius priced prescription in hand and I’m making my way back to my husband’s infusion room.
3:00pm – My husband has the IV fluids, magnesium, and an antibiotic finishing up and now they hook up the last antibiotic. I give him his mid-afternoon pills: Ibuprofen round #2 and Cellcept on an empty stomach round #2. I ask about hooking up with CMV infusion. They make me do it because they’re not allowed to touch it. I’m basically a nurse now. The CMV meds make Jeff nauseous so I give him a Zofran. #ZOLTAN

4:15pm – Now that the daily infusion is complete, we make our way over to the IV team to have his clogged PICC line looked at. I hope they can get it unblocked because he’s had a PICC line or port in every part of his body and the only place left is to put an IV in his groin. I saw a mere diagram drawing of this groin catheter situation in a catheter class and nearly passed out.
5:20pm – It’s freedom o’clock. Can’t wait to get home and watch some Forensic Files. I wheel Jeff back down to MD Anderson’s first floor and pay $15 for valet. The wait time is 20 minutes. We wait for what feels like an eternity. Every time someone coughs I think about how Jeff will eventually succumb to pneumonia because of this very moment. I’m not in a great place. Maybe the reason I watch Forensic Files because life is unfair and hard but at least I’m not getting murdered??
5:45pm – Our car pulls up and I tip the valet 2 bucks. They’re always super nice and I don’t think they get tipped often. Honestly, though, people with cancer are paying for $22,000 for a measly pocket full of life tic tacs, so I get it.
6:00pm – We shuffle back to our apartment and our dog loses her mind with excitement. She pees a little bit on the floor, which is unfortunate because we have carpeting. I’ll have to steam that later. I take her outside before there’s more than just pee on the carpet. It’s hard to be mad at someone who is so excited to see you that she pees a little bit. I go back upstairs to steam the carpet.

(throwback to a pre stem cell nap)
6:30pm – I steamed that section of the carpet with antibacterial because, if you weren’t aware, my husband has cancer. No laundry today because I did it yesterday. Go me. I’m basically a 1950’s housewife. And a nurse. Except I forgot about dinner which is rapidly approaching and, unlike a 1950’s housewife, I can’t cook.
7:30pm – I make something like a CPK pizza. Jeff’s taste buds are coming back and he is super pumped about it. Even if he wanted something super healthy, like a salad, he can’t have it until day 100 because raw foods could literally kill him at this point. Thank God we’re in Houston because this would not fly in Los Angeles. I remember to take out the CMV Chemo from the fridge this time.
8:45pm – We’ve finished eating. I want to Netflix and chill but I should probably shower. I have enough dry shampoo in my hair that I resemble a 17th century judge.
9:30pm – I flush Jeff’s PICC line and administer the CMV Chemo. I wait for it to finish and then flush it with Heparin. We keep the blood thinner companies in business, so I give him his second Lovenox injection of the day.
10:00pm – I give the dog a night time walk and, once back in the apartment, I wash my hands at an OCD level. I give Jeff his night time medicines: Cellcept, Ibuprofen, and Colace. I also give him a Dilaudid or Ativan if he’s in a lot of pain and can’t sleep. Mostly, that’s not a problem because fatigue is a side effect of about 18 of the medications he’s taking. He doesn’t sleep as much as he enters a light coma.

10:30pm – We’ve done it. We’ve made it through our first day home post transplant! Maybe now I’ll watch FOUR HOURS of 48 Hours Mystery with my headphones and my laptop light on the lowest setting in bed next to Jeff tonight. I check my MyMDAnderson appointments page to find out our infusion time tomorrow. It’s 6:00am. I shut my laptop and throw it in the trash.
Chemo: What to Expect When You’re Expecting Mostly Nausea

Before I had personal experience with chemo, movies and TV led me to believe that the nausea was the most traumatic part of it. Apart from losing your hair – but, wigs! Fun! Right, Samantha!?

In reality, what Jeff experienced was a myriad of things. He refers to this cluster of uncomfortable side effects as a “hangover times ten”.
TYPES OF CHEMO
There are many different types of chemo and they all look different. The first chemo Jeff was given was Doxorubicin, which chemo patients call the red devil (thanks for giving it this super chill, non threatening nickname!) because it looks like bright red Kool Aid.
Some chemotherapy drugs are clear. Some are given through an IV, and some require a patient to have a port or a picc line put in.
THE MEDICAL STAFF WILL LOOK TERRIFYING
Nothing rattles the nerves of a first time chemo patient like seeing the nursing staff bring over a chemo bag like it’s a scene in the movie Contagion. Everything is labeled hazardous to boot. The nurses handle so much chemo a day that they simple cannot be exposed at all to it, so they wear gloves, a gown, and a mask.

Chemo hasn’t advanced in a very long time, so if you can find any comfort in this, just know that the chemo you are about to receive has likely been used to cure many people since the 1950s.
NAUSEA
Jeff only had nausea once, on the first day of chemo, and that was because he hadn’t been prescribed a high enough dose of Zofran. Zofran got FDA approval in the 90s and it’s incredible. I also can’t hear the name without going, “ZOLTAN!”
Zofran completely gets rid of nausea for Jeff. That being said, all bodies are different. Some people respond better to a medication called Phenergan, or an anti nausea medication supplemented with something else like a sedative called Ativan. If something isn’t working for you, don’t be afraid to try things until you do. There’s no reason to be miserable. Even if you’re a masochist, it’s not worth spending the little energy you have (it’s needed for healing!) on tolerating a side effect.
WAIT FOR IT…
You don’t feel the effects of chemo immediately. I remember the first day of Jeff’s chemo. We watched the liquid move out of the bag, into the IV line, and slowly up into his port, watching as if it would hit his chest and he’d suddenly morph into a werewolf.

The most he felt was brain freeze from all the ice he was eating to deter mouth sores. It was anticlimactic. A few days later we saw the effects. It always happens around the same time white cell counts bottom out.
OTHER COUNTS WILL DROP, TOO
Expect hemoglobin and platelet count to drop along with the white blood cell count. This is normal, but low hemoglobin and platelets require transfusion if they drop below a certain amount. Every hospital/doctor has a different number requiring transfusion, but for MD Anderson it’s Hemoglobin under 8.0 and platelet count under 20.
MOUTH SORES
These are THE WORST. If you’ve ever had a cut in your mouth or a canker sore, it’s like that but imagine about 70 of them in your mouth at one time. You can’t eat, so be prepared to have smoothies. And not with too much fruit because – guess what – fruit juice irritates the sores. FUN.
MUCOSITIS
I call mucositis mouth pain on cocaine. The mouth sores were bad during the initial chemo but Jeff didn’t have mucus production. After myeloablative chemo (the most intense chemo) Jeff required suction at his bedside. The bucket would fill almost daily. It’s intense and does not subside until your white blood cell counts recover.
Clearing out mucus production is constantly like this:
And leaves you talking like Christian Bale as Batman for a couple of weeks after.
You hear a lot about chemo but not about the other medications that supplement the chemo. You may also have to take:
STEROIDS which cause HUNGER
Some chemos require steroids because of their T Cell repressing qualities. Steroids make you very emotional and hungry. Hangry or, as I call it, Chemotional.

When our doctor first gave my husband the steroids, I was the one he gave the warning to. “This could make your husband irrational. We’ve seen people throw things at their spouses.” His advice was basically to duck. Apart from eating an entire sleeve of cinnamon rolls at 6AM, Jeff never did anything completely irrational. He did get into an argument with someone he didn’t know on Facebook that I might have instigated circa Trump election. Jeff on steroids was mostly just like me on my period.
NEUPOGEN / NEULESTA which cause BONE PAIN
Once you’ve had chemo you’ll have an injection in your arm or stomach with a bone marrow stimulant. This will help your body quickly get new white cells in action. The quicker your white cells rise, the less likely you are to have an infection. It’s important to avoid infections at all costs. Also see: face masks below.
OPIOIDS which cause CONSTIPATION
All of the pain management drugs cause constipation, including a lot of anti nausea drugs. Chances are that if you’re having chemo you’re going to take something that causes constipation. Sure, it isn’t fun to talk to your doctor or anyone else about, but the consequences are serious. I talked to a stem cell doctor who lost three young male patients from bacteria introduced via enema. Medications used to counteract constipation (such as colace and miralax) do not have an IV form. If you have mucositis and can’t swallow, this leaves you vulnerable. Regularity is so important that you’ll go from someone who’s never peed with the door open to being like

PORT ISSUES
Ports often get tangled or kinked inside the body. Something as simple as a cough can coil the line inside the chest. Having to go in and have the port fixed is nerve wrecking, but it’s a common occurrence I’ve found in patients. Having procedures done to correct the port might happen a fair amount during your treatment. Jeff had a port inserted and then about a month later doctors had to do a procedure where they went up through the groin to pull a kink down. Then, after additional issues, the port had to be removed and another one placed on the other side of his chest. Very scary when you’re dealing with low blood counts because, again, risk of infection.
FACE MASKS

(not this kind)
Infections can be deadly. No night out to dinner or the movies is worth risking organ failure. That’s why, even when Jeff’s white cell counts were normal, he’d wear a face mask out at all times. We also took extra precaution and kept our distance from people who were around lots of other people. Children were no-nos. Think about all of the other children a kid comes in contact with at school and then those germs/bacteria are brought into your home at the end of the day. What I’m saying is – bathe your kids in Purell.
Don’t risk shaking hands. Remember to disinfect your cell phone. Be nice to people…from a distance.
Caregiving 101

It’s time to take care of yourself.
That’s probably not how you saw this post starting out. The entire point of caregiving is to care for someone else, not yourself. You’ve probably come to terms with the sacrifices you’ll make. You’re already imagining yourself saying things like, “this Oatmeal Cream Pie is fine for dinner”, “I don’t have time for feelings when there are so many things to do”, or “this bench I’m sleeping on at the hospital is killing my neck but my husband may or may not be dying so who cares!”
I went into caregiving the only way I knew how: Non Stop like Liam Neeson. For an entire 3 out of 12 months in 2016 I lived in a hospital room. Short term stays, long term stays, I’ve done them all. And I mostly didn’t give a shit because I grew up watching Nickelodeon GUTS, preparing for my own personal Aggro Crag and doing anything it took to get to the top.

Except it wears on you and before you know it you’re hooked up to a heart monitor yourself. I’m not being dramatic, that’s just what losing 12 pounds in two months followed by quickly gaining 6 of it back in vending machine foods will do to you. I’m on beta blockers now but I’m still fiercely worried about this:
Is Broken Heart Syndrome Real?
Everyone will push you to take care of yourself but it feels almost impossible, so I’ll lay out some things here that you can do for yourself.
PLANNER / NOTEBOOK / HOLE PUNCH
You’re going to get an Erin Brockovich level of paperwork to deal with. You’ll feel compelled to throw it away. DO NOT throw anything away. Nothing holds people accountable like a binder with facts. Bring a hole punch with you into the hospital to show staff you’re not here to mess around.

Learn how to read your blood work and don’t be afraid to ask questions. At UCLA, everyone hated when I had questions but I asked them anyway because I probably have PTSD and don’t trust anyone. Some doctors don’t like when you’re too involved but good ones will always want you to understand your body. When I first started asking questions I could see the look on their faces: I was a wife with Google and a case of denial, but guess what? It wasn’t denial, it was a hunch. And that’s what saved Jeff from complying to their treatment and getting sicker. Always double check things and ask questions. This one’s for your mental health and their physical health.
FIND AN EASY WAY TO GIVE PEOPLE UPDATES
I spent so much time updating people individually in the first few months that it was like I’d gone on a silent retreat where all I did was text. Save yourself the time and set up a page where you can post updates from the beginning. If you’re also looking to raise money for healthcare you can do this all in Go Fund Me, or if you’d like to keep it private you can use CaringBridge.org. You can also set up a Facebook group (which you can make public or private).
PACK A BACKPACK
Have a backpack packed and ready to go for last minute ER trips. Underwear, pajama pants, a clean shirt, a travel toothbrush, toothpaste, a sweatshirt, one of those airplane neck pillows, and a snack (like a granola bar). ER trips happen with a quickness. All it takes is a sudden “I feel warm” and seconds later you’re looking at a 101.5 Degree fever. Nothing says ‘from the house to the car in one minute flat’ like the fear of sepsis – and with a pre-packed backpack that minute includes calling someone to watch your dog. If you’re thinking a snack is overkill, sometimes you’ll go into the ER thinking it’ll be something “quick” like a transfusion (4-5 hours) and other times you’ll be admitted for days of testing but you won’t get an inpatient room (aka no food) for 8-10 hours. Basically, always have necessities and comfortable items on hand.
DRESS LIKE A BASIC BITCH
Speaking of comfortable, no one knows it like a basic bitch. In the beginning I’d bring jeans along to the hospital stays to change into. That didn’t last so long. Nothing says “hospital pro” like slippers/Ugg boots and stretch pants combo.

Don’t stop with basic-ing yourself. Basic your husband, too. Ugg slippers for men. Stop cringing. These bad boys protect your heels when you’re heading for a collision with your IV pole. Boxers. Soft ones. Dare I say…silk? Stop cringing. Sorry to bring up Ugg again, but this robe.
GET GOOD SLEEP
This is easier said than done. If you’re in the ER, you have an awful recliner. If you’re someone who is doomed to only sleep on their side (me), this is a real problem. You’re going to want to remember that airline pillow in the backpack. For longer term hospital stays (like for stem cell transplant), bring a cot like THIS ONE. It’s light enough to carry on your own and you can set it up to sleep right next to the hospital bed so you can be the sleeping equivalent of a couple who sits on the same side of the booth at a restaurant.

The REI cot is much better to sleep on. The cushioned benches are just as hard as you’re imagining and if you’re over 5’9, forget about it. My feet stuck out of the side. I can finally imagine what Abe Lincoln felt like.
Bring a couple of your own blankets and a pillow, depending on how finicky you are with sleep. The hospital pillows are essentially gauze stuffed with tissue paper, but if your neck is made out of whatever Gumby is, you’ll be okay.
SET YOURSELF UP FOR MENTAL STABILITY
I’m talking about a support system on speed dial. If you need to see a therapist and can’t leave your loved one, there’s an app called Talkspace where you can text with a therapist in your own time.
Anti depressants. If you’ve struggled with depression, now is the time to have a plan. In a run-of-the-mill month I could fight my way through a depressive slump but having my husband depend on me both physically and mentally didn’t leave much room for depression. I went on Zoloft for the first time in my life and even my husband noticed a difference in my ability to cope.
FOR LONGER TERM HOSPITAL STAYS
Puzzles. Adult coloring books. DVDs… But make sure they don’t have cancer or death in them if you’re at capacity. Cancer and death are super hot in Hollywood right now.
A white board to stay motivated. Put goals on it (activity/meals/medications to remember) and display it in a place that will push and remind you.

Keep your life in your peripheral. Nothing moves healing faster than thinking about the good things in the future. There’s this company called Fathead I used to make peel off murals that they’d allow in the hospital room. Our puppy is directly where my husband can see her.

TRY A LITTLE TOO HARD BECAUSE WHO CARES YOU’RE GOING THROUGH CANCER
Twinkle lights. These are 18 dollars. Powered by 2 AA batteries. Ambiance.
A Fitbit – this is a great way to check your loved one’s heart rate when they’re off heart monitor and you’re awake and watching them breathe and wishing you knew what their heart was doing because you are a hypochondria ridden basket case.
Toilet paper that doesn’t suck. This actually could go up in necessities but I don’t like to pretend I know what other people’s butts require. What I do know is that the hospital toilet paper is probably what the hospital pillows are stuffed with, so not the best quality.
A foam roller – you can get one small enough to pack in a suitcase here. This really helps when you’re sitting/standing in one room most of the day.
Foods you can nuke. I like to rotate Rice A Roni and those little cups of Velveeta mac and cheese with actual food. If you’re going to be at MD Anderson there are coffee stations but they take $2.50 in quarters. This is why I’m at the Starbucks in my basic bitch outfit twice a day, so if you spot me please feel free to stop me and ask me about my husband’s cancer.