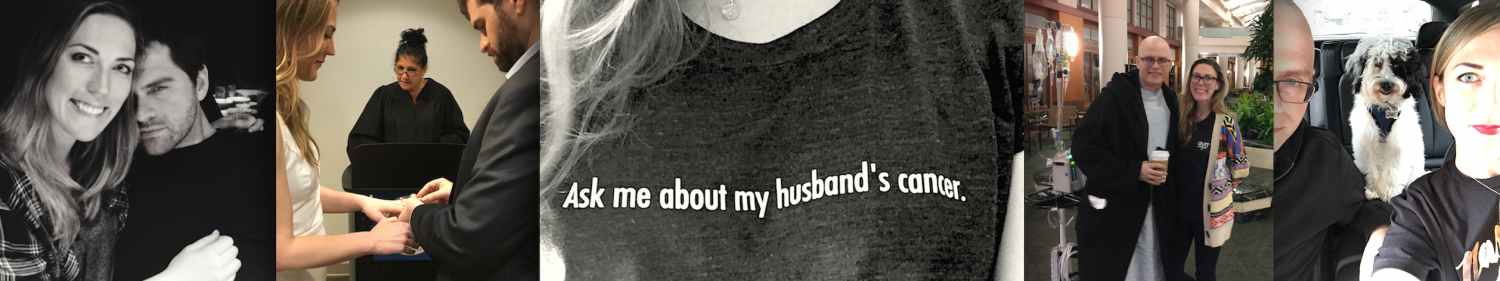
I asked my BFF for advice on being there after a cancer diagnosis because she handled it like a champ.
What To Do When You Find Out Your Friend Has Cancer
by Brandy Finmark
Cry. Stare at a wall. Start to text some of your close friends and family the news while crying onto your phone but then cancel the text because even that feels like it takes too much energy. Stare at a wall some more. Question reality. Robotically start doing laundry even though all of your clothes are clean because your mind is clearly handling this well. Do more menial tasks like organizing your desk or counting how many books you actually own. Is it enough to make you seem smart but not enough to make you look like you don’t watch TV? Start crying again because you’re thinking about your fucking image and now you’re comparing yourself to a Kardashian. Try to watch TV but just end up staring through it. Lay on your couch. Stare at a wall. Realize you forgot your laundry in the washing machine. Decide you’re never leaving your house or wearing clothes again because what’s the point of anything?
There’s nothing that can prepare you for getting horrible news. No handbook that tells you how to deal with a cancer diagnosis for someone close to you. When my best friend called me and told me her husband had been given 10 months or so to live, and he’s only 34 and they’re just 3 months married, you don’t know how to react. I sat on the other end of the phone, trying not to cry too hard, and let her talk as much or little as she needed. No matter how well you know someone, this person suddenly feels like a stranger. One you have no idea how to comfort or communicate with. Like after a break up with someone you’ve been with for years; they suddenly seem so far and distant from you and you have no idea what to say to them or how to act. Once we got off the phone, I remember thinking, “did I do enough? Was that okay? what can I do? Should I go to the hospital? Should I bring her something? Should I make her laugh? Make her laugh? What’s wrong with you? Are you a serial killer?”

A few days after the initial shock, the reality of the situation sets in. Not only is your best friend; who you spend more time with than any boyfriend you’ve ever had; going through something no 31 year old should go through, but also this man, who’s become your close friend, too, is going through something no 34 year old should ever have to go through. The doctor’s had given him a diagnosis of a rare cancer called Angiosarcoma, which the google search for basically just says “SORRY BRO”. How can you process that? Denial. That’s how!
Quickly after the diagnosis, they had to go to a sperm bank before the chemo started two days later. I couldn’t stop thinking how fucking horrible it was that these two beautiful people, who just started their life together, have to now freeze his sperm if they ever want children. Then I couldn’t stop thinking about the fact that my friend had to get turned on enough to provide a sperm sample in a cup the day after he’d been told by life:

How did that sperm donation even go? Was my best friend in there with him? Did she have to turn him on? That was the second time I realized I was probably a serial killer. Who fucking thinks about that?? I DO. I guess the only reason I’m talking about it is because sure, it’s a weird thought to have. But when we’re in these situations and our brains are at max capacity of comprehension, sometimes they go to weird places, so you shouldn’t feel bad if you find yourself wondering about the details of your friends’ sperm donation.
After the sperm donation, they prepared to start chemo to extend his life expectancy. No matter how well you know someone, you’re never quite sure how they’re going to handle grief or what it is you can do for them. Everyone needs something different in these situations, and all you want to do is help in any way you can. There’s also no way of knowing how you, yourself, are going to handle the changes that happen. You go from talking to and seeing your friend all day, every day, to only talking when they can muster up words. As the friend of someone going through this, you go through your own small “grieving” period. Grieving your life as it was less than a month ago. You feel like a selfish piece of shit because you shouldn’t be wishing your life was back to normal, but I think that’s normal. How would I know? I’m mostly a serial killer.
I really struggled with how to be there for them. What I could do for them. I’d offer so many things and then feel like I was annoying them by offering so much. One night, I was talking to a friend and telling her I wasn’t sure if I was doing enough, and she said, “all you can do is be there for them. That’s it.” And I realized she was right. That’s the only thing I could do. I didn’t have to keep sending things or hiring maids to clean their house or bringing over food or searching the black market for organs I could give them in case it helped… I mean, all of those things are great. But the number one thing I could do was be there whenever either of them needed me. And mostly, it was to vent. Talk. Sort through whatever horrible shit was going through their brains. The thing I had to work through was my response of how to fix it. I’m a fixer. I like to fix things.

But I went against my instincts and instead of offering up solutions to her problems, I just fucking listened. I shut my dumb mouth and listened. And listened. And listened some more. And I realized how much that helped. Listening is the number one thing you can do for anyone who’s going through a horrible situation. Unless they’re on fire. Then throw a blanket or some water over them because listening won’t do shit. You’re welcome.
After a couple of weeks of feeling out what it is they needed from me, I figured out what it is I would do to be there and help:
A) Text her daily that I love her. Even if it annoyed her. The one thing I’ve heard is how lonely this can be to go through, so I just wanted both of them to know I was here, even if I wasn’t there. Also, text him funny gifs or air hugs. And that I loved him.
B) Let them know I was available to come over and bring food or movies whenever they needed. Not push it, just let them know. Then, anytime they invited me over, I’d cancel anything I had going on and be there.
C) Do things that aren’t asked of you. Clean their house, buy groceries, walk their dog. Basically just do anything you can think of that might make their life a little easier.
D) Balance being emotional and light. I made sure to be positive and upbeat when I was around them. I didn’t want him thinking he was being pitied, because no one likes that. I also sat and watched my friend cry, and I would cry with her. I would balance my crying so I was never crying MORE than her because don’t be a selfish dick. But it’s okay to show emotion. Cry. Hug. And you can never say “I love you” to someone you love too many times in this situation.
That was how I was going to move forward. In the coming weeks and months, I did all of those things as often as I could. And guess what? Your own life DOES move on. You have “small dramas” in your own life. Dating drama, friend drama, family drama. And you want to talk to your best friend, who always knew how to help you. You get sad that person isn’t available to help you through things. But you have to realize that friend is going through something you don’t understand. And they probably don’t have the capacity to deal with what’s going on in their own life, let alone yours. Their whole life has been turned upside down and you want to talk about the guy who didn’t call you back after 3 dates? Not that your problems aren’t problems, but just have some perspective. In times like these, your job as a friend is to be there for them. I’m sure you have other friends. And those friends will be the ones you go to for advice. Also, it helps to have a friend you can talk to about this situation, because you’re going to be sad and feel helpless and that’s okay. Just make sure you talk to someone else about it because again, don’t be a dick.
A couple of months after the initial diagnosis, the doctor’s realized they had misdiagnosed him. I KNOW. The new diagnosis was still cancer, and still a rare form, but this one gave him a shot. It went from 0-50%. It’s a weird thing when you’re actually EXCITED about a cancer diagnosis, but when you hear NO to MAYBE you’re all:

Since then, my friends moved from LA to Houston to get treatment at MD Anderson. They have an apartment right next to the hospital, and have been in and out for treatments and appointments. It’s been about 4 months from the initial diagnosis and a couple of months since the new diagnosis. I think at this point, it’s easy for friends to “move on” with their life, and stop being as available. The immediacy sort of goes away. People care, obviously, but they have their own lives to get back to. I, on the other hand, have a unique situation where I’m incredibly single and alone and probably have an unhealthy love and affection for these two people and have nothing but time. I’m like a stalker without the restraining order. So I’m available to be more available. But when this is happening, remember that your friends are in this, day in and day out. It doesn’t just go away because you’ve finally come to terms with it and have decided you have to live your life. I mean, you do. I’m not saying quit your job and move in with them, but please remember to send them a text, or post something nice on their Facebook page, or send them a cancer singing-gram.

This is a shitty situation. Never forget that it’s SHITTIEST for the person diagnosed with the cancer, and that they’re actually the ones fighting for their life, but it’s still a horrible situation for everyone involved. At times, you’ll feel overwhelmed. You’ll feel bad living your own life and having a good time when you remember that your friends are in and out of hospitals, living every day fighting to live another. You’ll listen to your friend and watch them go through every emotion, sometimes in one sitting. You’ll feel like you still aren’t doing enough. But you are. As long as you’re there for them when they need to talk. As long as you make sure and remind them that you’re thinking about them and they’re not in this alone. As long as you can clear room in your own schedule to make time to go be with them. If that means flying to Houston, then you fly to Houston.
This is a process. A long, arduous process that takes a huge emotional toll on all of the people going through it. So try and remember to show up for them. At the end of the day, that’s all you can do. That, and drink. A LOT. But not too much because what if your friends need you and you’re too drunk to answer the phone??? (That’s literally a huge worry for me but you live your life). Be good to yourself. Be healthy. Be grateful you have your health. And remind your friend, whose health is ailing, that soon, they’ll have their health back, too. And also, fuck cancer. Fuck it real hard.







 (the only pyramid scheme I’m interested in)
(the only pyramid scheme I’m interested in)