Sometime back in 2016 I found myself reading posts like this one. I was searching for information but, blog after blog, I’d stumble across the feared update: their person didn’t make it. This blog is no exception. My husband passed away on March 17th, 2019, while waiting for a liver transplant.
It’s important that those of you reading this and looking for answers understand – this is not your outcome. Ours does not foreshadow yours, even if you have the same cancer by name. Every cancer and every body is genetically very different. It’s always worth giving your all in the fight to live.

I have a constant need for information. With cancer, it was all so that we could make the best decisions about Jeff’s treatment. I didn’t think there would be any decisions weighing on me if it ever came to Jeff’s passing. I wouldn’t even let it enter my mind. But now I know that Jeff’s passing only happened the way it did because I’d become friends with so many others who had lost their loved ones. They’d shared their experiences with me. Because of them, I knew what to fight for when the time came. I’m so grateful for them. I’m grateful that Jeff and I were able to have the best possible final moments together in what I would otherwise call the worst time of my life.
If you’d rather not think about the worst case scenario, I understand, but if you would rather know, I’m going to share some of the things that prepared me. The transition is hard enough without wishes and regrets.

Chances are, you’ll know when the time is coming. Jeff entered the ICU on February 27th and I was told that he wouldn’t be alive through the weekend. I instinctively knew that wasn’t true. He was with me until March 17th.
If you’ve been with someone through treatment you’ll probably have a hunch. I’ve talked to others who have had similar intuition. This intuition can give you the time to fight for the really important things, like when to stay and ask for certain liberties (which I’ll get to in a minute).
Jeff needed to be intubated the following day but the staff were casual about it. I was told he’d likely be off intubation and talking again by the following day but I didn’t know how unlikely that actually was. I tell you this because there’s the possibility you’ll have a last moment to communicate and you won’t realize it. Our last words were “I love you” before he was sedated. I had no idea they would be the last words he’d ever speak. A single moment can end up being the most significant.

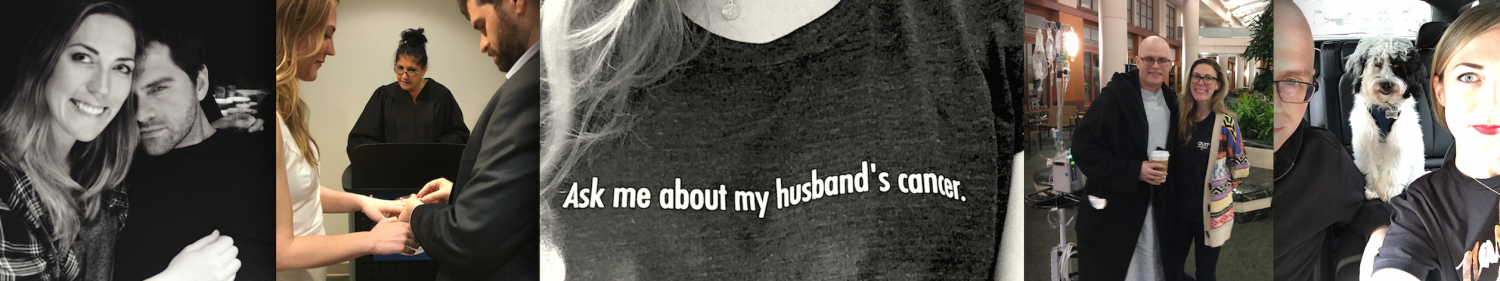
Over the next few weeks, Jeff was essentially in a comatose state but open eyed. This same thing happened to other friends who have passed from cancer. Efforts to communicate go in and out with their eye movements and hand squeezing. No one knows how well people in this state are able to comprehend, but I had signals from Jeff that he was listening and aware. Talk to your person. Play their favorite music. Give them as much contact as you can. Now is a good time to mention: nurses will probably ask that you don’t sleep in the room but you can bypass this by sleeping sitting up in the same chair that would be in there regardless. You can find creative ways to sleep so that you can stay. Sleeping in the lounge does not give you good rest anyway (see pictured below). Everyone will try to get you to leave the hospital and rest, but I look back and I’m glad I stayed every moment that I could.

Medical staff will likely want to do testing while in the ICU to try to resuscitate. A lot of tests are invasive and painful, and a lot of times your person can’t say they’re in pain. Sometimes you can see it on their faces. Pain medication can lower blood pressure (in other words, destabilize the body) so they don’t like to use it, but there are medications like Versed you can ask for. They’re thinking about resuscitating and not comfort, so it’s always good for the caregiver to keep being aware of how comfortable they look.
Cardioversion / defibrillation is where they shock your heart back into normal rhythm. Jeff had this twice. It’s not a rare occurrence in the ICU and absolutely doesn’t mean death but it is frightening to watch. If you’re in the ICU for any extended period of time you’re going to see your fair share of cardioversion and, unfortunately, death. In the 3 weeks we were in the ICU I happened to see 4 people pass. There isn’t a way to emotionally prepare for it, but you can expect it.
 (note found in the ICU guest bathroom)
(note found in the ICU guest bathroom)
Be nice to the nurses. They have the ability save lives just as much as the doctors. One of Jeff’s nurses brought his body temperature from 92 degrees to normal by engineering her own way to warm dialysis bags. This gave us extra time to try to resuscitate him, and for new doctors to make rounds. Changing doctors can be a good thing. We went from having one doctor who said he refused to do cardioversion if Jeff required it, to another doctor who constantly read papers to come up with new ideas on how to recover his blood flow.
And finally: fighting for the really important things. Jeff’s blood pressure steadily began dropping on the morning of the 17th. I knew it would only be a matter of hours. I asked the nurses to help move him closer to one side of the bed so that I could lay with him but, because of various infections acquired in the hospital, they didn’t want me to have that much contact with him. The hospital takes this sort of thing seriously but I refused to take no for an answer. You have to push back. They’re doing their jobs but this is something that will be with you for the rest of your life and doing what’s right in a loved one’s final moments is more important than any system. If you want something specific like this, your best bet is to find someone on staff to have your back. I was lucky to have a doctor on my side. He let me lay next to my husband so he didn’t go through it alone.

I can’t reiterate how much the final moments can impact you. Try to go easy on yourself. Start therapy as soon as you can, try to find a grief specific therapist. There are groups like Our House where you can meet other spouses / siblings in your age group (I find this to be important) in similar situations. If an in-person group isn’t really your thing, my friend Nora started The Hot Young Widows Club where you can ask anything and everything online.
But even with various resources and incredible friends and family, grief can sometimes feel like an island. That’s because cancer has a way of deepening your love before taking them from you. Cancer makes sure you see someone at their very core and then, when they’re gone, the grief is what is left. At Jeff’s celebration I talked about how we fit 30 years into the last 3. I talked about how most couples would be lucky to get the same amount of time we did in a whole lifetime, but the reality is I was lucky to find Jeff at all.

He gave me more love than most people receive in a lifetime. I’ll hold on to that forever.

No matter how long it’s been since my last post, please don’t hesitate to reach out to me. If anything that Jeff and I went through can be helpful to you, I’m happy to talk about it. I can add it to the long list of beautiful reasons we were given this life together. So please keep asking me. Ask me about my husband’s cancer. Ask me about loss. Ask me about life. JessicaRBlackwell@gmail.com

This was so beautiful and informative. I lost my aunt to Glioblastoma and there were a lot of similarities in terms of fighting for last moments. Our family, four years later, obviously changed forever, is doing well. I’m glad your voice is out there. Not everyone could express this stuff in such a comforting way.
LikeLike